RAISING GOOD CHOLESTEROL DOESNOT PREVENT TUBERCULOSIS
*
Prof Dr,DRAM,HIV /AIDS,HEPATITIS ,SEX DISEASES & WEAKNESS expert,New Delhi,India, +917838059592
Raising HDL, widely known as good cholesterol, for years has been thought to protect against heart attack and stroke. But a big new study published Monday found little evidence it does.The finding upends the advice doctors have been giving millions of patients — and helps explain why the drug industry has failed time and again, despite billions in investment, to develop a drug that cuts deaths from heart disease by boosting HDL levels.
“When you explain [cholesterol levels] to patients, it’s very easy to say one number’s bad and the other number’s good,” said Dr. Dennis Ko, a cardiologist at Canada’s Institute for Clinical Evaluative Sciences and lead author of the study. But it turns out that HDL is associated with poor health generally and does not seem to affect cardiovascular risk.
These pricey cholesterol drugs aren’t selling. And that has the biotech industry sweating
Instead, it dipped, then hit a plateau; people with HDL of about 40mg/dL had roughly the same risk as those with about 80 mg/dL. And death risks actually increased for those with extremely high levels of good cholesterol.
Further muddying the picture, people in the low-HDL group were also more likely to die of diseases unrelated to the heart. And they had lower incomes, higher body weights, and poorer diets than others in the study, all of which correlate with increased mortality on their own.
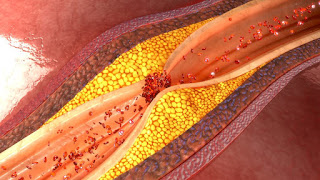
HDL has been thought to lower cardiovascular risk by cleansing the bloodstream of “bad” cholesterol and scrubbing the inner walls of blood vessels, so your levels of HDL were thought to predict your risk of heart attack or stroke. But this new data suggests HDL may just be a fatty substance along for the ride.
The study, published in the Journal of the American College of Cardiology, will sound familiar to the drug industry, which has repeatedly failed to design a pill that might improve patients’ lives by increasing HDL.A decade ago, Pfizer spent more than $800 million to get the HDL-boosting medication torcetrapib into late-stage trials, only to find that more patients died on the drug than on placebo. Roche was next to fail when its drug, dalcetrapib, came up short in a 16,000-patient trial in 2012. And last year, Eli Lilly shut down a study testing its evacetrapib on 12,000 patients after discovering that the drug had no effect on heart attack and stroke.
Those drugs, called CETP inhibitors, are meant to interrupt the process that turns HDL into LDL cholesterol, its “bad” relative. And, in a sense, they work — Lilly’s pill boosted HDL by about 130 percent and slashed LDL by more than one-third. But, time after time, changing that ratio of good to bad cholesterol has failed to improve outcomes for patients.
Still, cardiologists said it may still be useful to keep measuring HDL in blood lipid tests, because it does seem to be correlated with other factors that can affect health, such as diet and exercise habits. Doctors can gather such information with questionnaires, but those are time-consuming and rely on patients accurately recounting their habits.
- Kidney stones universally present hazard in north india,dillution by water prevent it
- Steroid and placebo effect equally for mild persisting asthma with low sputum eosinophils
- Government wants to fix public healthcare staff shortages with ayush docs: will it work?
- Plea in hc for payment of salaries of edmc, north mcd teachers and doctors
- 7 indian pharma companies named in us lawsuit over inflating generic drug prices
- Woman in up dies after explosion in her mouth during treatment,what is diagnosis?
- Woman in up dies after explosion in her mouth during treatment,what is diagnosis?
- Woman in up dies after explosion in her mouth during treatment,what is diagnosis?
- Air pollution ! mothers organising rally in london,anaesthetist choosing gas,will india follow?
- Cardiac arrest is always not sudden as understood -a study




 Comments (
Comments ( Category (
Category ( Views (
Views (